Low-level laser/light therapy (LLLT) is one of the most important treatments I have used to restore my brain function after serious concussions, toxic mold exposure and multiple psychiatric prescriptions.
And in my experience, it is one of the most efficient ways to boost brain function and improve mental health.
Yet your doctor likely has no idea what it is.
It’s about as cutting-edge as it gets, and even more unconventional than neurofeedback. But it works.
Also known as photobiomodulation, LLLT is the application of low-power lasers or light-emitting diodes (LEDs) to the body for therapeutic purposes. When LLLT is applied to the brain, it is known as transcranial LLLT or transcranial photobiomodulation (44).
LLLT has been around since 1967, and there are now more than four thousand scientific studies showing that it can help treat a variety of disorders without any harmful effects. Unlike high-intensity surgical lasers, low-powered lasers do not cut or burn tissue. Instead, these lasers stimulate a biological response and encourage cells to function properly (11, 12, 33).
And luckily, it’s very easy to treat yourself at home with LLLT using red and infrared light.
I use three main devices on my brain and they have significantly improved the quality of my life.
Make sure you read the Recommended Devices section below, where I discuss the different devices I use.
How It Works
Research shows that red and infrared light between the wavelengths of 632 nanometers (nm) and 1064 nm produce positive biological effects. For brain cells, the optimal range appears to be between 800 nm and 1000 nm, as these wavelengths can penetrate the scalp and skull and reach the brain (19, 20, 25-31).
The devices I use fall within this range.
The light emitted from the devices below stimulate a photochemical reaction within cells, which can accelerate the natural healing process and cause beneficial changes in behaviour (45).
How does it do this?
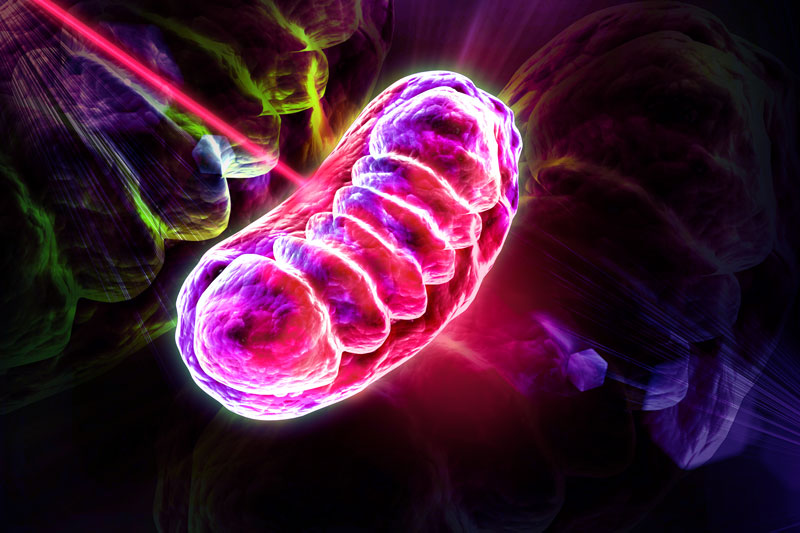
Mainly by supporting your mitochondria.
As I’ve discussed before, mitochondria are considered the “powerhouses of the cell,” generating most of the energy in your body in the form of adenosine-5’- triphosphate (ATP).
ATP is your body’s main source of cellular fuel. You are constantly using it, and your brain needs enough of it to work properly.
Proper mitochondrial function and ATP production is critical for neuroprotection, cognitive enhancement, and the prevention and alleviation of several neurological and mental disorders (46).
And research demonstrates that transcranial LLLT supports mitochondrial function and significantly increases the production of ATP in the brain (3-5, 8-10, 13-17, 21-22, 34, 45).
Your mitochondria contain photoacceptors that absorb the photons from light and convert them into ATP – energy that can be used to perform cellular tasks and biological processes (39, 40).
This process is comparable to plant photosynthesis, during which sunlight is absorbed by plants and converted to energy for the plants to grow (23, 24).
By stimulating the mitochondria and producing more ATP, LLLT gives brain cells extra ATP energy to work better and heal and repair themselves.
On top of this, LLLT has also been shown to:
Increase neurogenesis, brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF) (1, 41, 42)
Reduce inflammation (1, 35, 37, 41)
Decrease free radicals and oxidative stress in the brain (2)
Increase blood flow and circulation, including within the frontal cortex (6, 18, 32)
Reduce pain by increasing our body’s endorphins (natural opioids and natural pain relievers) (7, 36)
Increased rate of oxygen consumption in the frontal cortex (32, 100)
Increase serotonin (38)
My Experience and What You Should Expect
Along with neurofeedback, LLLT is one of the most impactful actions I have taken to optimize my brain and mental health.
By the time I was off all psychiatric medications, I had lost a lot of my full cognitive capabilities. Thankfully, LLLT has restored them.
Here are some of the results I’ve noticed:
Increased cognitive function
Sharper thinking
Improved mood, concentration, alertness
Less fatigue and reduced need for sleep
More mental motivation, endurance and productivity
Overall, it has improved my mental constitution. I don’t get fatigued and worn down as easily and I can focus and think harder for longer periods of time.
LLLT also has a cumulative effect. Your brain becomes stronger and more resilient over time as you do the treatment consistently.
It has allowed me to reduce the number of supplements I take daily. I now realize that I needed the treatment for many years, but I just didn’t know it existed.
Luckily, I’m now able to treat myself on a regular basis and I’ve never felt better.
Many serious brain injuries and mental illnesses can be successfully treated with LLLT, including depression, anxiety, post-traumatic stress disorder, traumatic brain injury, post-concussion syndrome, stroke and Alzheimer's disease.
I explore how LLLT has been shown to help each of these disorders below. Feel free to skip to the disorder you're struggling with to learn more.
Depression and Anxiety
Studies in rats and humans provide evidence that LLLT improves mood and decreases depressive symptoms.
In 2009, researchers took 10 patients with a history of major depression and anxiety (including post-traumatic stress disorder and substance abuse) and applied LLLT to their foreheads for four weeks. At the end of the study, six of the 10 patients experienced a remission of their depression, and seven of the 10 patients experienced a remission of their anxiety. There were no observable side effects (54).
“The data supports that LLLT to the head constitutes a promising neurotherapeutic tool to modulate behaviour in a non-invasive manner.”
This makes sense considering that several studies show that depression is linked to abnormal blood flow in the frontal cortex of the brain, and LLLT increases blood flow and circulation (47, 53).
Other studies have shown that participants report a significant increase in positive emotions and a reduction in depressive symptoms for two weeks after LLLT treatment (55-57).
Sufferers of traumatic brain injury (TBI) also experience a decrease in depression, anxiety, irritability and insomnia, and an overall improvement in quality of life, because of LLLT (58, 59).
I’ve personally experienced all of these results.
Traumatic Brain Injury
Traumatic brain injury (TBI) is a growing health concern. An estimated 1.7 million people sustain a TBI annually in the U.S. (60).
Mild TBIs (concussions) make up 75 per cent of all brain injuries. Military personnel deployed to Iraq and Afghanistan frequently experience mild TBI while overseas, and many months after they return home, they often struggle with PTSD, depression and anxiety (61, 62).
And research shows that transcranial LLLT can help (63).
I personally experienced this. In 2010, I suffered multiple concussions while living in a moldy home, and thankfully LLLT has helped me completely recover from post-concussion syndrome. It’s helped me as much as neurofeedback.
A number of human studies show that patients with chronic mild TBI experience improved cognition, memory and sleep with LLLT treatment.
One study examined whether LLLT could help 11 patients with chronic mild TBI symptoms. They all had cognitive dysfunction, and four of them had multiple concussions like I did.
After 18 LLLT sessions, their cognition, memory and verbal learning improved. Participants also said they slept better and had fewer PTSD symptoms. Coworkers, friends and family reported improved social, interpersonal, and occupational functioning (65).
If LLLT was a drug, we would definitely be hearing about it.
In another study, 10 people with chronic TBI were given 10 treatments of LLLT (810 nm) and witnessed a reduction in headaches, cognitive dysfunction, sleep problems, anxiety, depression and irritability (66).
There have also been a few case studies showing beneficial effects of transcranial LLLT in TBI patients (67, 68):
“Seven years after closed-head TBI from a motor vehicle accident, case 1 (a 66-year-old woman) began transcranial LED treatments. Before LLLT treatment, she could focus on her computer for only 20 minutes. After eight weekly LLLT treatments, her focused computer time increased to 3 hours. She has treated herself nightly at home for 5.5 years now and maintains her improved cognition at age 72 years.”
“Case 2 (a 52-year-old retired, high-ranking female military officer) had a history of multiple closed-head injuries. Before beginning LLLT treatments, she was on medical disability for 5 months. After 4 months of nightly LLLT treatments at home, she returned to working full-time as an executive consultant with an international technology consulting firm and discontinued medical disability. Neuropsychological testing performed after 9 months of transcranial LED showed significant improvement in cognition and memory, as well as reduction in post-traumatic stress disorder symptoms.”
“Case 3 received 20 LLLT treatments over two months and experienced highly favourable outcomes with decreased depression, anxiety, headache, and insomnia, whereas cognition and quality of life improved.”
So LLLT can improve cognition, reduce costs in TBI treatment and be applied at home?
Hmm, sounds like something the pharmaceutical industry would not like people to know about – and something that would force them to lose a lot of life-long customers.
Several mouse studies also show that transcranial LLLT can prevent cell death and increase neurological performance after TBI (69-72).
Researchers believe that LLLT works so well for people struggling with TBI symptoms because mitochondria in the brain are significantly dysfunctional after TBI, resulting in an inadequate supply of ATP, and LLLT can support the mitochondria and increase ATP production (73-75, 79).
There is also poor blood flow and oxygenation, and increased inflammation and oxidative stress in the brain after head injuries. This contributes to brain damage, but LLLT can help combat these problems, increase antioxidants, promote neurogenesis and relieve chronic symptoms (76-78, 80-83).
Alzheimer's Disease and Cognitive Impairment
Research shows that LLLT can boost performance and improve cognitive function, including attention and memory, in elderly people, young healthy people and animals.
Preliminary studies demonstrate that LLLT could slow down the progression of Alzheimer’s disease by decreasing a protein in the brain that is linked to dementia (84-86, 94).
Downregulation of brain-derived neurotrophic factor (BDNF) occurs early in the progression of Alzheimer's disease, and LLLT has been shown to prevent brain cell loss by upregulating BDNF (87).
“LLLT could be used as a preventive intervention in people who present risk factors for Alzheimer’s disease, mild cognitive impairment, or a history of head trauma. In such patients, LLLT could be combined with cognitive intervention approaches.”
Researchers have also applied LLLT to middle-aged mice, and discovered that the memory and cognitive performance of the middle-aged mice improved so much that it was comparable with that of young mice. The researchers concluded that LLLT should be “applied in cases of general cognitive impairment in elderly persons” (5, 88).
Several others studies have shown that LLLT significantly increases alertness, awareness and sustained attention, and improves short-term memory and reaction time. Study participants also made fewer errors during tasks and tests (89-91, 93, 95).
Another study found that LLLT was just as effective as exercise at enhancing cognition, likely by providing neuroprotection and supporting the mitochondria (92, 96).
Stroke
Multiple studies show that LLLT can significantly reduce brain damage and improve recovery outcomes after a stroke (110-113).
In one study, researchers applied LLLT over the entire surface of the head of stroke patients approximately 18 hours after a stroke. Five days after the stroke, they found significantly greater improvements in the LLLT-treated group. The improvements continued 90 days after the stroke. At the end of the study, 70% of the patients treated with real LLLT had a successful outcome compared with only 51% of the control subjects (114).
Follow up studies with over 600 stroke patients found similar beneficial results. Researchers believe increase in the production of ATP is responsible for the improvements (115, 116, 117).
Numerous studies also show that LLLT significantly reduces neurological problems and improves behaviour in rats and rabbits after stroke. It also increases the growth of new brain cells in these animals, improving their overall recovery (118-124).
Other Disorders
There are a number of other disorders that can also improve with LLLT treatment:
Parkinson’s disease (PD) – “Mitochondria in PD tissues are compromised, and LLLT could be developed as a novel treatment to improve neuronal function in patients with PD” (109).
Amyotrophic lateral sclerosis (ALS) - Mitochondrial dysfunction and oxidative stress play an important role in motor neuron loss in ALS. Motor function significantly improved with LLLT in a group of people in the early stage of the disease (99).
Autism – Linked to mitochondria dysfunction and inflammation, so LLLT would likely help (103, 104).
Bipolar disorder – Linked to mitochondria dysfunction and inflammation (105, 106, 107)
Schizophrenia – Linked to mitochondria dysfunction and inflammation (105, 106)
Smoking Cessation – Check out this video.
Alcoholism (101, 102)
Opiate addiction (102)
Headaches and migraines (108)
Acne - This is unrelated to brain health but LLLT can also treat acne. Improving my diet and gut health helped me overcome my acne, but I definitely wish I had known about LLLT when I had it. An integrative physician I know has had a lot of success with her patients struggling with acne and other skin issues (97, 98).
Recommended Devices
I first discovered LLLT when reading Dr. Norman Doidge’s book, The Brain's Way of Healing: Remarkable Discoveries and Recoveries from the Frontiers of Neuroplasticity.
Dr. Doidge talks about the BioFlex Laser Therapy equipment, which costs tens of thousands of dollars.
I found an integrative physician who owned a Bioflex and I gave it a try.
After a few sessions, I started experiencing beneficial effects.
So I decided to go ahead and buy my own LLLT devices for much cheaper.
I ended up finding and trying a number of different LLLT devices myself
They were much less expensive than the Bioflex, and I wanted to see how they compared to the Bioflex.
Many of the devices I bought didn't help me very much because they weren't powerful enough.
Most light devices aren't very effective at penetrating the skull.
But after a lot of research, and trial and error, I found devices that were powerful enough.
And they did help me.
And they provided me with the same brain and mental health benefits as the expensive Bioflex.
Here are the three devices I now recommend because they actually work:
Optimal 1000 Brain Photobiomodulation Therapy Light (Combo Red/NIR) - This is a powerful device that shines 660 nm of red light and 850 nm of infrared light. I shine it on my forehead for 5 minutes every day. I also shine it on other parts of my head and on my entire body, including on my thyroid, thymus gland and gut. I experience incredible benefits from doing this.
Optimal 300 Brain Photobiomodulation Therapy Light (Combo Red/NIR) - This is a smaller and more convenient device that I take with me when I’m travelling. I shine it on my forehead.
Vielight Neuro Duo – This is a transcranial-intranasal headset with 810 nm of near infrared light that I’ve now been using regularly. It penetrates deeper into brain tissue and is absorbed better by the central nervous system. If you decide to get this one, you can use the coupon code JORDANFALLIS for a 10% discount. Some research has shown a 20-fold higher efficiency of light delivery to the deep brain through the nose instead of transcranial application (125). Vielight has several different devices and you can also use the coupon code JORDANFALLIS for 10% off any of them.
Unlike most pharmaceuticals, LLLT is very safe, non-toxic and non-invasive, so you can easily try it on yourself without concern and see if it helps you like it has helped me (33, 34, 126).
You can shine the light all over your head. But start slow and apply the light to different areas of your head for just 1-2 minutes, maybe even less if you’re really sensitive. Then work your way up to longer periods of time, perhaps 5-10 minutes per area. There’s no exact proper way to do this. Listen to your body and see how it affects you.
It’s important to note that some people experience grogginess and fatigue after using LLLT. I experienced this the day after my first treatment. I was incredibly tired and lethargic. This was a sign that I did too much.
If you feel extremely tired immediately after LLLT or the next day, take a break and do less next time. For example, if you applied light to your forehead for 3 minutes, then drop back down to 2 minutes for your next session.
It is also important to cycle LLLT. The way it works is similar to exercise, so you need to take breaks in order to heal and get stronger. Using it everyday can cause a burnout effect. I use it every other day to give my brain a chance to recover.
More Details on How I Use the Optimal 1000 Therapy Light
Someone recently asked me for more details on how I use the Optimal 1000 Brain Photobiomodulation Therapy Light (Combo Red/NIR). So I thought I’d share what I told them here:
I usually hang the Optimal 1000 Brain Photobiomodulation Therapy Light (Combo Red/NIR) on my door, and then start by standing in front of it for about 10 minutes. I would say I'm about 1 or 2 feet away so that the light is shining on most of my body. I tend to prioritize my upper body though, particularly my thyroid, gut, thymus gland, and of course my head. But what I've found is that shining it on other parts of your body (besides my brain) actually leads to indirect cognitive benefits as well. So it's not just shining it on the brain that helps with cognitive function.
I will also sometimes turn my back to the light and shine it on my back and spine area, and on the back of my head, for about 5 to 10 minutes.
I also get much closer (perhaps about 2-3 inches away) and shine it just on my forehead for 4-5 minutes or so. It is safe to do this because our devices emit a very low, safe level of EMFs.
So what I usually do is 10 minutes on my entire body and then right after that, 5 minutes on my face/forehead. But it's completely fine to do them separately at different times of the day or on completely separate days if you want.
It's usually good to limit your exposure to a maximum of 20 minutes at a time though, because too much at one time can make you too tired and negate the beneficial effects.
The back of your head where your spine meets your skull is another great area to shine the light. I also like to shine the light on the sides of my head (around my ears) for a few minutes each.
Conclusion
Frankly, it’s ridiculous that this therapy is not more well-known and promoted by doctors. But like everything else on this website, you don’t have to wait for conventional medicine to catch up, and you can experiment with the LLLT devices yourself. There is a high benefit-to-risk ratio.
I suspect that home-use application of LLLT will become much more popular in the coming years.
The remarkable effects of the treatment in healing the brain in a non-invasive manner, along with the fact that there is little evidence of any adverse side effects, suggests to me that it’s use will only increase.
At the same time, distrust in pharmaceuticals continues to grow because of uncertain efficacy and unbearable side effects.
And as the Western population continues to age, the incidence of the degenerative brain diseases will only continue to increase, which will produce a severe financial and societal burden.
So people will realize they are at a disadvantage by not having their own device(s) and will start using them on a regular basis for optimal mental health and cognition.
I've come to this conclusion, and I'm glad I did.
References:
(1) http://www.ncbi.nlm.nih.gov/pubmed/23003120
(2) http://www.ncbi.nlm.nih.gov/pubmed/23281261
(3) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3945284/
(4) http://www.ncbi.http://www.ncbi.nlm.nih.gov/pubmed/21274733lm.nih.gov/pubmed/21274733
(5) http://www.http://www.ncbi.nlm.nih.gov/pubmed/22850314.nlm.nih.gov/pubmed/22850314
(6) http://www.ncbi.nlm.nih.gov/pubmed/15954817
(7) http://onlinelibrary.wiley.com/doi/10.1002/lsm.20583/abstract
(8) http://www.ncbi.nlm.nih.gov/pubmed/9421973
(9) http://www.ncbi.nlm.nih.gov/pubmed/11959421
(10) http://www.ncbi.nlm.nih.gov/pubmed/17603858
(11) http://www.ncbi.nlm.nih.gov/pubmed/5098661
(12) http://www.ncbi.nlm.nih.gov/pubmed/4659882
(13) http://www.ncbi.nlm.nih.gov/pubmed/10365442/
(14) http://www.ncbi.nlm.nih.gov/pubmed/6479342/
(15) http://www.ncbi.nlm.nih.gov/pubmed/2476986/
(16) http://www.ncbi.nlm.nih.gov/pubmed/17463313/
(17) http://www.ncbi.nlm.nih.gov/pubmed/19837048/
(18) http://www.ncbi.nlm.nih.gov/pubmed/19995444/
(19) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2442599/
(20) http://www.sciencedirect.com/science/article/pii/S0004951414601276
(21) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3288797/
(22) http://www.ncbi.nlm.nih.gov/pubmed/23239434?dopt=AbstractPlus
(23) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3953713/
(24) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065857/
(25) https://www.ncbi.nlm.nih.gov/pubmed/26535475
(26) https://www.ncbi.nlm.nih.gov/pubmed/26347062
(27) https://www.ncbi.nlm.nih.gov/pubmed/24568233
(28) https://www.ncbi.nlm.nih.gov/pubmed/21182447
(29) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2796659/
(30) http://stroke.ahajournals.org/content/40/4/1359.long
(31) https://www.ncbi.nlm.nih.gov/pubmed/17463313
(32) http://www.medscape.com/viewarticle/775815
(33) https://www.psio.com/pdf/LLLT-of-eye-and-brain.pdf
(34) http://www.ncbi.nlm.nih.gov/pubmed/6200808
(35) http://www.ncbi.nlm.nih.gov/pubmed/22275301
(36) http://www.ncbi.nlm.nih.gov/pubmed/17439348
(37) http://www.ncbi.nlm.nih.gov/pubmed/17868110
(38) http://www.ncbi.nlm.nih.gov/pubmed/26202374
(39) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3288797/
(41) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065857/
(42) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538543/
(44) http://www.ncbi.nlm.nih.gov/pubmed/25772014
(45) http://www.ncbi.nlm.nih.gov/pubmed/19837048
(46) http://www.sciencedirect.com/science/article/pii/S0006295213007417
(47) http://www.ncbi.nlm.nih.gov/pubmed/15025051
(48) http://www.ncbi.nlm.nih.gov/pubmed/16043128
(49) http://www.ncbi.nlm.nih.gov/pubmed/12946880
(50) http://www.ncbi.nlm.nih.gov/pubmed/15061044
(51) http://www.ncbi.nlm.nih.gov/pubmed/15570642
(52) http://www.ncbi.nlm.nih.gov/pubmed/12181629
(53) http://www.ncbi.nlm.nih.gov/pubmed/10739143
(54) http://www.ncbi.nlm.nih.gov/pubmed/19995444
(55) https://www.ncbi.nlm.nih.gov/pubmed/27267860
(56) http://dose-response.org/wp-content/uploads/2014/06/Gonzalez-Lima_2014.pdf
(57) https://www.ncbi.nlm.nih.gov/pubmed/23200785
(58) https://www.ncbi.nlm.nih.gov/pubmed/26535475
(59) https://www.ncbi.nlm.nih.gov/pubmed/26347062
(60) https://www.cdc.gov/traumaticbraininjury/pdf/bluebook_factsheet-a.pdf
(61) http://www.ncbi.nlm.nih.gov/pubmed/18234750/
(62) https://www.cdc.gov/traumaticbraininjury/pdf/mtbireport-a.pdf
(63) http://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0053454
(65) https://www.ncbi.nlm.nih.gov/pubmed/24568233
(66) https://www.ncbi.nlm.nih.gov/pubmed/26347062
(67) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3104287/
(68) https://www.ncbi.nlm.nih.gov/pubmed/26535475
(69) http://www.ncbi.nlm.nih.gov/pubmed/17439348/
(70) http://www.ncbi.nlm.nih.gov/pubmed/19800810/
(71) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538543/
(72) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3397203
(73) http://www.ncbi.nlm.nih.gov/pubmed/11059663
(74) http://www.ncbi.nlm.nih.gov/pubmed/19637966
(75) http://www.ncbi.nlm.nih.gov/pubmed/16120426
(76) http://www.ncbi.nlm.nih.gov/pubmed/18501200/
(77) http://www.ncbi.nlm.nih.gov/pubmed/19995444/
(78) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3397203/
(79) http://www.ncbi.nlm.nih.gov/pubmed/17439348/
(80) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3397203/
(81) http://www.ncbi.nlm.nih.gov/pubmed/17439348/
(82) http://www.ncbi.nlm.nih.gov/pubmed/17439348
(84) http://www.ncbi.nlm.nih.gov/pubmed/18769048/
(86) http://www.ncbi.nlm.nih.gov/pubmed/24994540
(87) http://www.ncbi.nlm.nih.gov/pubmed/23946409
(88) http://www.ncbi.nlm.nih.gov/pubmed/17855128/
(89) https://www.ncbi.nlm.nih.gov/pubmed/23200785
(90) https://www.ncbi.nlm.nih.gov/pubmed/27080072
(91) https://www.ncbi.nlm.nih.gov/pubmed/26017772
(92) https://www.ncbi.nlm.nih.gov/pubmed/27220529
(93) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3953713/
(94) http://www.ncbi.nlm.nih.gov/pubmed/24387311
(95) http://www.sciencedirect.com/science/article/pii/S1074742707001153
(96) http://www.ncbi.nlm.nih.gov/pubmed/23806754
(97) http://www.ncbi.nlm.nih.gov/pubmed/22615511
(98) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3352636/
(99) http://www.ncbi.nlm.nih.gov/pubmed/19143012/
(100) https://www.ncbi.nlm.nih.gov/pubmed/26817446
(101) http://www.ncbi.nlm.nih.gov/pubmed/15674998/
(102) http://www.ncbi.nlm.nih.gov/pubmed/19995444
(103) http://www.ucdmc.ucdavis.edu/publish/news/newsroom/8932
(104) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3554862/
(105) http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0004913
(106) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3626880/
(107) http://www.ncbi.nlm.nih.gov/pubmed/23196997
(108) http://www.ncbi.nlm.nih.gov/pubmed/12811613
(109) http://www.ncbi.nlm.nih.gov/pubmed/19534794/
(110) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538543/
(111) http://www.ncbi.nlm.nih.gov/pubmed/19995444
(112) http://www.ncbi.nlm.nih.gov/pubmed/17463313/
(113) http://www.ncbi.nlm.nih.gov/pubmed/19233936/
(114) http://www.ncbi.nlm.nih.gov/pubmed/17463313/
(115) http://www.ncbi.nlm.nih.gov/pubmed/19233936/
(116) http://www.ncbi.nlm.nih.gov/pubmed/20425181/
(117) http://www.ncbi.nlm.nih.gov/pubmed/19837048/
(118) http://www.ncbi.nlm.nih.gov/pubmed/19995444
(119) http://www.ncbi.nlm.nih.gov/pubmed/16946145/
(120) http://www.ncbi.nlm.nih.gov/pubmed/17693028/
(121) http://www.ncbi.nlm.nih.gov/pubmed/17678491/
(122) http://www.ncbi.nlm.nih.gov/pubmed/16444697/
(123) http://www.ncbi.nlm.nih.gov/pubmed/17693028
(124) http://www.ncbi.nlm.nih.gov/pubmed/15155955